Revolution and Evolution at Widener University’s Healthcare Management Alumni Association 2016 Annual Meeting
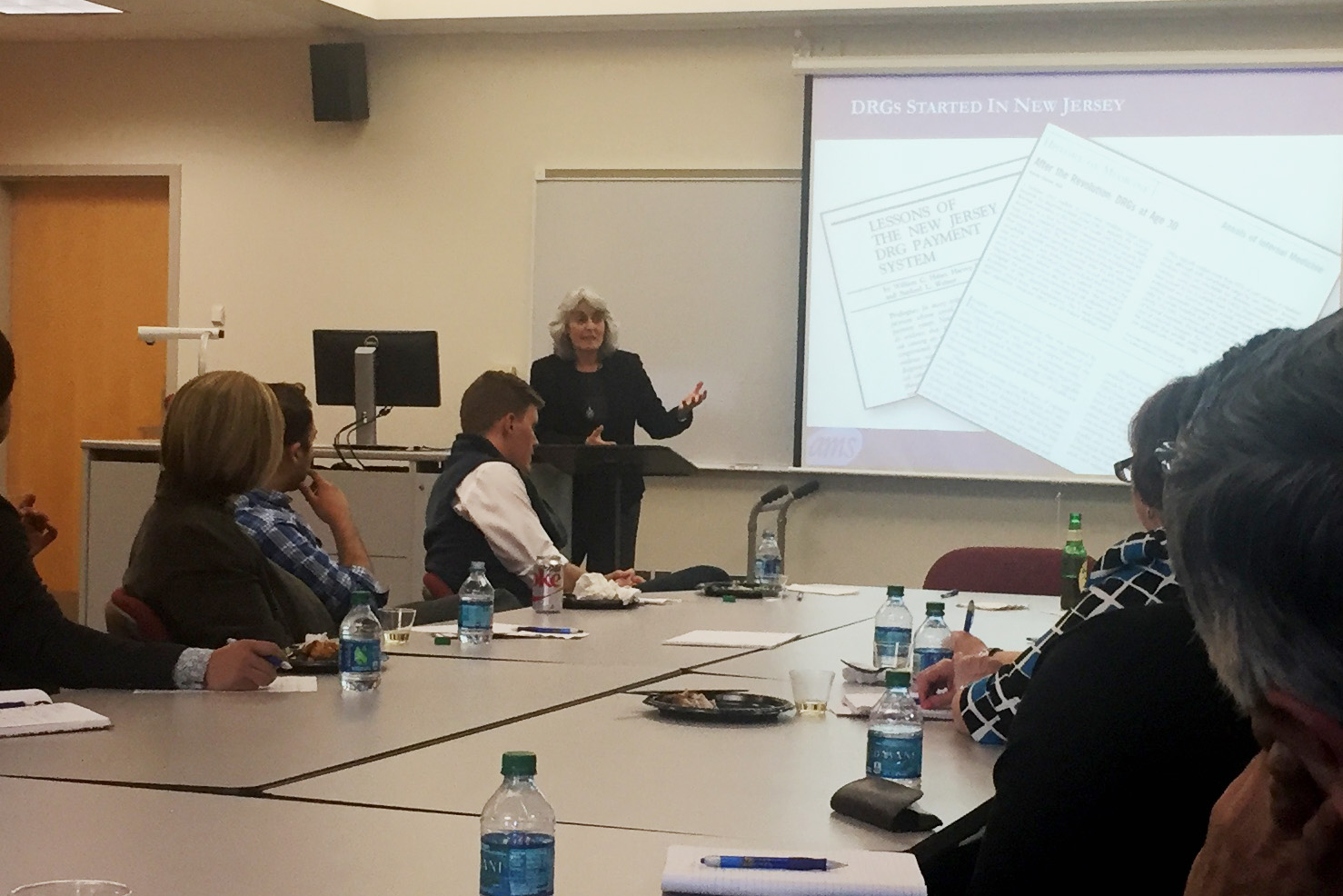 At the April 2016 annual meeting of Widener University’s Alumni Association for its Graduate Program in Healthcare Management (Chester, PA), AMS President Jo Surpin presented how payment approaches changed since the formation of DRGs in New Jersey in the early 1980s in a talk called: “Revolution and Evolution: How the Gainsharing Model Aligns Physician and Hospital Incentives”. Jo detailed how the lessons learned of the NJ DRG payment system were carried through to the Federal DRG program, and then how gainsharing discussions started at the end of the 1990s, leading to CMS demonstration projects as well as very successful commercial gainsharing programs offered by state hospital associations.
At the April 2016 annual meeting of Widener University’s Alumni Association for its Graduate Program in Healthcare Management (Chester, PA), AMS President Jo Surpin presented how payment approaches changed since the formation of DRGs in New Jersey in the early 1980s in a talk called: “Revolution and Evolution: How the Gainsharing Model Aligns Physician and Hospital Incentives”. Jo detailed how the lessons learned of the NJ DRG payment system were carried through to the Federal DRG program, and then how gainsharing discussions started at the end of the 1990s, leading to CMS demonstration projects as well as very successful commercial gainsharing programs offered by state hospital associations.
 Attending the session was Michael D. Rosko, PhD, Professor of Health Care Management at Widener University. Dr. Rosko’s research interests over the years has led him to examine how hospitals respond to cost containment initiatives such as the Medicare Prospective Payment System and Certificate of Need regulations; payment policy by HMOs; and financial pressures associated with uncompensated care.
Attending the session was Michael D. Rosko, PhD, Professor of Health Care Management at Widener University. Dr. Rosko’s research interests over the years has led him to examine how hospitals respond to cost containment initiatives such as the Medicare Prospective Payment System and Certificate of Need regulations; payment policy by HMOs; and financial pressures associated with uncompensated care.
At the Widener Alumni Association meeting, Dr. Rosko critiqued the AMS gainsharing approach using the following method for evaluating payment systems based on several academic sources:
Payment System Evaluation Criteria |
Gainsharing based on Internal Cost Reduction |
| Promote the efficient production of services by providers | Encourages efficiency. By incenting physicians to decrease inpatient costs, the resources used to treat inpatients are decreased. |
| Provide for equitable payments from purchasers (i.e., no cost shifting but there should be adjustments for severity of illness) | Does not impact payor payments, so costs are not shifted among payers. Costs are evaluated based on APR DRGs, so incentives are calculated reflecting case-mix and severity of illness. |
| Provide a level of reimbursement to providers that will maintain their viability | Provides for loss of income that physicians may experience by decreasing utilization. For example, medical physicians get reimbursed on a per-diem basis for inpatients. The gainsharing incentives include a component to compensate for length of stay reductions which compensate for the loss of income. |
|
Improve quality of care |
Links quality metrics to incentive payments, including institution-specific objectives |
|
Require minimal administrative cost |
No hospital has hired any additional staff to administer the program. The program also is integrated with other hospital initiatives to encourage physician engagement. There is an annual fee payable to the hospital association for administering the program. Participating facilities report that these costs are a very small fraction of cost reduction opportunity. |
|
Not subject to provider manipulation (no gaming of the system) |
Incentives are calculated by a third party independent scorekeeper (AMS) using a uniform methodology. The incentives are calculated based on a combination of:
|
The AMS gainsharing program clearly meets the criteria that Dr. Rosko outlined. The criteria also is helpful in evaluating other payment approaches, such as bundled payments, CJR, and ACOs. Below is a list of recommended readings from Dr. Rosko on these criteria:
- Rosko, Michael D. (1984, Spring). The Impact of Prospective Payment: A Multi-Dimensional Analysis of New Jersey’s SHARE Program. Journal of Health Politics, Policy and Law. 9(1): 81-101.
- Rosko, Michael D., Broyles, Robert, and Aaronson, W.E. (1987, Winter). Prospective Payment Based on Case-Mix: Will It Work in Nursing Homes? Journal of Health Politics, Policy and Law. 12, 683-701.
- Rosko, Michael D. and Mutter, Ryan. (2010, February). Inefficiency Differences between Critical Access Hospitals and Prospectively Paid Rural Hospitals. Journal of Health Politics, Policy and Law. 35(1): 95 – 126
- Rosko, Michael D. and Broyles, Robert. (1988). The Economics of Health Care: A Reference Handbook. New York, NY: Greenwood Press. Page 439.

Title: Professor
Organization: Widener University
Physician alignment with management initiatives is often difficult to achieve for a variety of reasons. When Jo Surpin and Anthony Stanowski first described gainsharing programs to me, my immediate reaction was that the incentives of this type of program should generate substantial physician buy-in. After learning more about gainsharing from Jo, other articles and Anthony’s blog I am even more convinced that this can be a useful tool in the quest to bend the cost curve. I really like the inclusion of adjustments for severity and the inclusion of quality/outcome metrics in the incentive mechanism. Gainsharing satisfies commonly accepted criteria for a good payment mechanism.